Prepare for Pediatric Head Injuries in the ED Around Halloween

Every year around Halloween, the number of head injuries spike in the ED. We want you to be prepared for Halloween-related head injuries, including the 5 specific injury patterns to be aware of from the Emergency Medicine section of our Pediatrics Core.
Prevalence of head injuries
Head injuries are common—especially this time of year! For all children, falls are the most typical cause of head injury, although motor vehicle trauma is the most common cause of serious head injury, and can also be more prevalent during Halloween time.
Symptoms to look out for
Symptoms to watch for include loss of consciousness, amnesia, vomiting, lethargy, headache, irritability, seizures, and behavioral changes (“not acting right”). Significant brain injury is not ruled out in the absence of signs of external head trauma!
5 specific injury patterns to be aware of
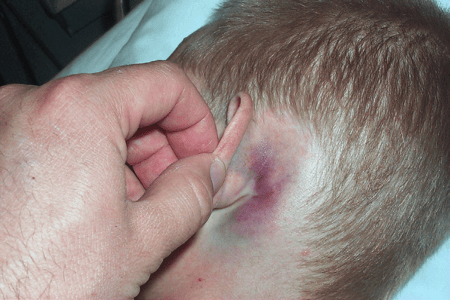
Basilar Skull Fracture
A fracture at the base of the skull, involving temporal bone, occipital bone, and/or ethmoid)
-
- “Raccoon eyes” (presents 1–3 days after injury)
- Battle sign (presents 1–3 days after injury)
- Hemotympanum
- CSF leakage from ear or nose (puts patient at risk for meningitis)
- Cranial nerve palsy
- Hearing loss
Racoon eyes and battle sign images—Source: Thomas Krzmarzick, MD
Abusive Head Injury
-
- Retinal hemorrhages
- Subdural hematoma (particularly subacute or chronic)—see next
- Other unexplained injuries
Subdural Hematoma
-
- Hemorrhage in potential space between dura and arachnoid membrane
- Caused by: nonaccidental trauma, fall from significant height, motor vehicle collision (MVC)
- Symptoms include headache, irritability, vomiting, lethargy, seizure, coma
- Crosses suture lines, not midline
Epidural Hematoma
-
- Hemorrhage from middle meningeal artery into space between dura and calvaria
- Caused by: fall from significant height, MVC, direct blow to temporal area
- Transient initial improvement in mental status (“lucid interval”) followed by headache, vomiting, lethargy, seizure, and coma
- Crosses midline, not suture lines (where dura tightly adheres to the skull)
- Needs urgent surgical intervention
- Minimal underlying brain injury, with survivors having a better long-term neurologic outcome than with subdural hematomas
Cushing’s Triad
Cushing's triad, representing increased intracranial pressure:
-
- Bradycardia
- Hypertension
- Hyperpnea and/or irregular respirations
Signs of severe head injury include marked alteration in level of consciousness, focal neurologic signs, posturing, dilated or unequal pupils, abnormal vital signs (especially bradycardia and hypertension), and scoring < 8 on the Glasgow Coma Scale. These children usually require intubation, as well as treatment directed at maintaining normal circulation/perfusion while lowering the increased intracranial pressure (ICP). Many have multisystem trauma, complicating their management. Be sure to protect the cervical spine until injury is excluded. Consult a pediatric neurosurgeon immediately or transfer to a pediatric trauma center with neurosurgical capabilities.
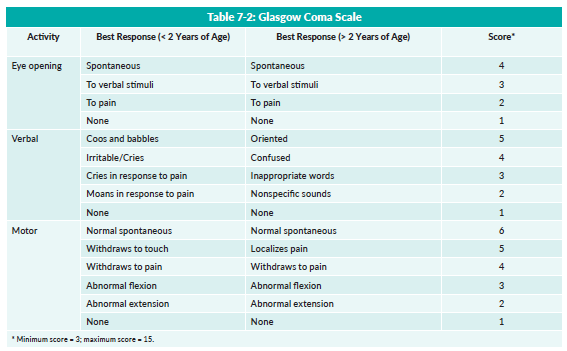 Glasgow Coma Scale from the Emergency Medicine section of our Pediatrics Core
Glasgow Coma Scale from the Emergency Medicine section of our Pediatrics Core
In the prehospital setting, the patient should not be moved and the C-spine should be immobilized unless the patient is lucid enough to cooperate with C-spine evaluation. If necessary, the airway can be maintained with a jaw thrust maneuver. Remember that unless properly performed, removing helmets or other sporting equipment results in C-spine movement; therefore, clothing and protective equipment should not be removed if at all possible.
Some other causes for ED visits around Halloween include:
- Animal bites from dogs protecting their homes
- Eye injuries from sharp objects that are part of Halloween costumes
- Dehydration from trick-or-treating
To brush up on these other Halloween-related injuries, make sure you flip or scroll through the Emergency Medicine section of the MedStudy Pediatrics Core!