If you follow us on any of our social accounts, you probably saw our #12DaysOfQandA posts. During December 1st–12th we posted one Q&A per day from our Internal Medicine Q&A bank or our Pediatrics Q&A bank to help our followers StudySTRONG during the holiday season!
Here's a recap of our 12 Days of Q&As!
Pro Tip: When looking through these Q&As try to dredge up all the info you can in your brain about that topic and question before looking at the answer. Studying Q&As like this helps you to remember them better.
Day 1 Pediatrics Q&A
On the second day of 12 Days of Q&As MedStudy gave to me.... A question from the Endocrine section of the Peds Q&As!
A 2-year-old female presents with a history of breast enlargement. She has no evidence of any androgen effects and has a normal growth rate. You suspect premature thelarche.
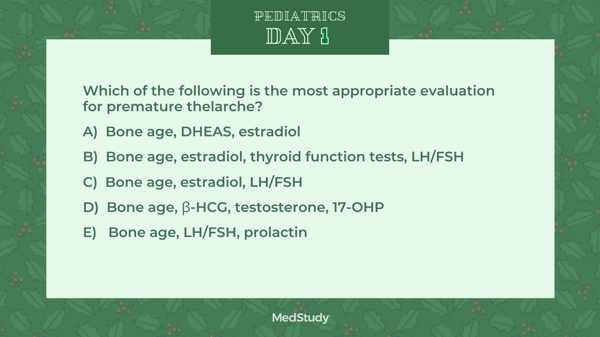
Answer is C: Bone age, estradiol, LH/FSH
Premature thelarche is defined as a patient with isolated breast development. Premature thelarche occurs in the first 2 years of life. Her evaluation would include breast development, a lump under her breast, or chest pain. On evaluation, her bone age would be within 2 standard deviations of her chronological age, and she would have no other signs of puberty. Her growth velocity would be normal. Her GnRH stimulation test would be FSH predominant (prepubertal), and she would have normal estradiol levels of < 10 pg/mL.
Appropriate evaluation and management would include asking about estrogen exposure during the history and, on the physical exam, concentrating on her growth velocity, Tanner stage, and skin exam. Appropriate initial lab and x-ray evaluation would include an estradiol, LH/FSH, and bone age.
Follow-up exams should be scheduled every 3–4 months. Further evaluation may include a head MRI, pelvic ultrasound, and GnRH stimulation test if the initial screen is abnormal and you are concerned with precocious puberty or ovarian pathology.
Day 2 Internal Medicine Q&A
On the second day of 12 Days of Q&As MedStudy gave to me.... A question from the General Internal Medicine section of the IM Q&As!
A 65-year-old woman is coming in for a routine physical examination. She is concerned about postmenopausal osteoporosis. She walks regularly and occasionally does a low-impact aerobics class.
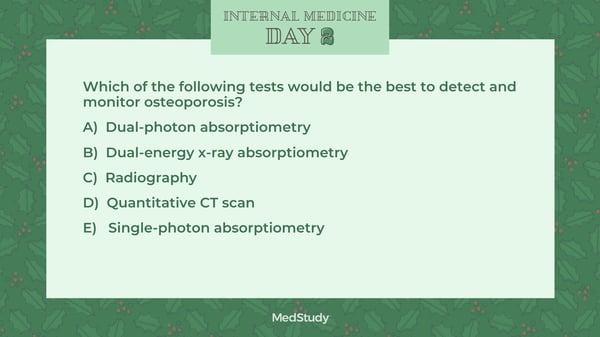
Answer is B! Dual-energy X-ray absorptiometry (DXA) uses an x-ray source, which means there is no radioactive decay (as seen in dual-photon absorptiometry) and energy stays constant over time. Hence, DXA has become the “gold standard” for bone mineral density measurement today. Scan times are also short, and the radiation dose is very low. DXA scans are extremely precise, with precision ranging between 1% and 2%.
Bone loss is only apparent on plain x-ray once about 40% of the bone is lost.
Single-photon absorptiometry (SPA) uses a single-energy photon beam that is passed through bone and soft tissue to a detector. The amount of mineral in the path is then quantified. SPA measurements are accurate, and the test usually takes about 10 minutes.
Dual-photon absorptiometry (DPA) uses a photon beam that has 2 distinct energy peaks. One energy peak is more readily absorbed by soft tissue, and the other is more absorbed by bone. The soft-tissue component is then subtracted to determine the bone mineral density. Although DPA is accurate for predicting fracture risk, precision is poor. In addition, the machine has limited usefulness in monitoring bone mineral density changes over time.
Quantitative CT (QCT) scan is unique in that it provides for true 3D imaging and reports bone mineral density as true volume density measurements. The real advantage of QCT is the ability to isolate an area of interest from surrounding tissues. However, the radiation dose with QCT is about 10× that of DXA, and QCT tests are more expensive than DXA.
Day 3 Pediatrics Q&A
On the third day of 12 Days of Q&As MedStudy gave to me.... A question from the Allergy and Immunology section of the Peds Q&As!
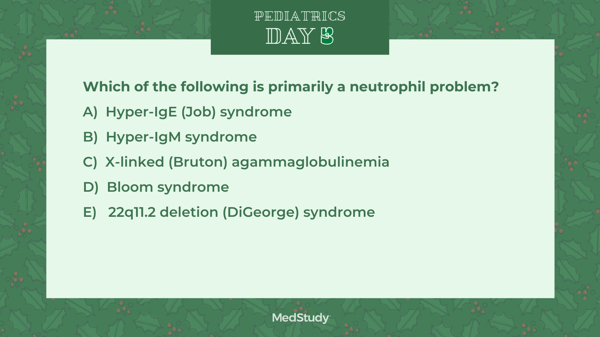
Answer is A: In hyper-IgE syndrome (a.k.a. Job syndrome), neutrophils fail to adhere to the endothelium and enter the tissues. Secretion of chemotactic chemokines and interleukins (e.g., IL-5 and IL-11) bring eosinophils to the tissues, with secondary stimulation of IgE production and the severe atopic picture of eczema. However, the primary neutrophil problem leads to deep abscesses, primarily with Staphylococcus aureus.
Hyper-IgM syndrome (a.k.a. CD40 ligand deficiency) is a problem of T-cell activation and subsequent failure of immunoglobulin isotype switching, leading to high IgM and low IgG and IgA. These patients have severe T-cell deficiency.
X-linked agammaglobulinemia (a.k.a. Bruton agammaglobulinemia) is a B-cell defect with low levels of all immunoglobulins.
Bloom syndrome is caused by a defect in the DNA repair machinery of the cell, leading to genomic instability and increased sensitivity to DNA-damaging agents. Patients also have reduced numbers of T cells.
Patients with 22q11.2 deletion syndrome (a.k.a. DiGeorge syndrome) have reduced numbers of T cells due to thymic aplasia.
Day 4 Internal Medicine Q&A
On the fourth day of 12 Days of Q&As MedStudy gave to me.... A question from the Rheumatology section of the IM Q&As!
-png.png?width=600&name=tw%20day%204%20(1)-png.png)
Answer is A- Tuberculous arthritis.
Inflammatory changes of synovial tissue are typically very nonspecific, and biopsy provides very limited information. An exception to this is septic arthritis due to tubercular organisms, for which synovial biopsy is the gold standard (synovial fluid cultures have a low diagnostic yield for tubercular organisms) for pathology and culture. Tuberculous arthritis typically presents as a chronic monoarthritis; hip and knee joints most commonly are affected.
Psoriatic arthritis is diagnosed based on a history of psoriasis and concomitant chronic inflammatory arthritis. In many cases, the psoriasis precedes the arthritis by ∼ 7–10 years.
Reactive arthritis is diagnosed when a patient presents with inflammatory arthritis and a history of a recent gastrointestinal or genitourinary infection (these include Chlamydia trachomatis, Yersinia, Salmonella, Shigella, Campylobacter, Escherichia coli, Clostridium difficile, and Chlamydia pneumoniae) or streptococcal pharyngitis.
Rheumatoid arthritis is diagnosed based on a history of chronic, symmetric (and usually smaller joint) inflammatory arthritis. The patients may also have positive autoantibodies (e.g., rheumatoid factor, anti-cyclic citrullinated peptide [CCP] antibodies) or erosive disease of the joints.
Crystalline-induced arthritis would be diagnosed best using synovial fluid analysis alone. Polarized light microscopy identifies gout and calcium pyrophosphate dihydrate crystals. Alizarin red staining identifies hydroxyapatite crystals (associated with a destructive arthritis [also referred to as “Milwaukee shoulder”] and characterized by a noninflammatory hemorrhagic fluid aspirated from larger joints such as the shoulder), as well as calcium oxalate crystals (seen in patients with chronic kidney disease). Synovial biopsy may yield a specimen that could be used to evaluate for crystals; however, synovial fluid aspiration/analysis is far less invasive and, as a result, is preferred.
Day 5 Pediatrics Q&A
On the fifth day of 12 Days of Q&As MedStudy gave to me.... A question from the Nephrology and Urology section of the Peds Q&As!
Late one night, a 16-year-old boy arrives in the emergency department complaining of 45 minutes of severe right testicular pain. He feels nauseous, denies trauma, and his exam reveals an absent cremasteric reflex.
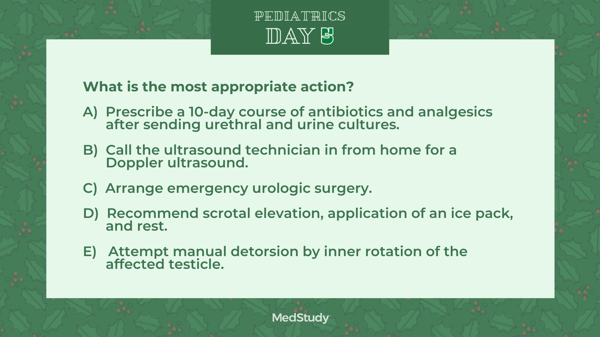
Answer is C: Arrange emergency urologic surgery.
This clinical vignette is most consistent with testicular torsion. Testicular torsion refers to the torsion of the spermatic cord and is a surgical emergency! The patient presents with acute onset of severe pain in the testis, the inguinalarea, and often the lower abdomen—commonly with accompanying nausea/vomiting. On physical exam, the affected testicle is diffusely swollen and tender; it typicallylies higher than the testicle on the contralateral side and in a horizontal rather than vertical plane. The cremasteric reflex is absent—the absent cremasteric reflex is the key to diagnosing testicular torsion. Absent cremasteric reflex is 100% sensitive but not as specific. A radionucleotide scan or color Doppler ultrasound demonstrates decreased perfusion in the scrotal images on the affected side.
Testicular torsion requires immediate surgical detorsion of the affected testicle with surgical fixation of both testicles (bilateral orchiopexy); salvage of the affectedtesticle is the rule if surgery takes place within 6 hours of onset of symptoms. The testicle remains viable in 60% of cases if surgery is performed within 6‒12 hours. Recovery of testicular function falls to about 20% if surgery occurs after 12 hours. Viability after 24 hours is rare.
Although there is a wide differential diagnosis for the acute scrotum, including several diagnoses that can be managed medically, it is an emergency if the cause of the pain is ischemia. To preserve the testicle, emergency surgery must be performed if the blood supply to the testicle is compromised.
Imaging of the testicle can be very helpful but must be done within 60 minutes of the onset of pain and should not delay surgical correction. Since the affected testicle typically rotates inwardly, manual detorsion can be attempted through rotating the testicle in an outward direction. An attempt at manual detorsion should not delay an emergent call to a urologist, however.
The patient’s clinical findings are consistent with testicular torsion, which is a urologic emergency. Antibiotics, as would be prescribed in the treatment of epididymitis, are not indicated.
Symptoms of epididymitis can be relieved with scrotal elevation, an ice pack, and rest. Symptoms of testicular torsion are not relieved with scrotal elevation.
Day 6 Internal Medicine Q&A
On the sixth day of 12 Days of Q&As MedStudy gave to me.... A question from the Hematology section of the IM Q&As!
-png.png?width=600&name=day%206%20tw%20%20(1)-png.png)
Answer is C - Testicular cancer
Hematopoietic stem cell transplantation (HSCT) has emerged as a potential definitive therapy for a wide variety of malignant and nonmalignant conditions. Common indications include hematologic malignancies, including leukemia, lymphomas (Hodgkin’s and non-Hodgkin’s), and multiple myeloma (as consolidative therapy after induction for clinically fit patients). Other nonhematologic uses include relapsed testicular germ cell cancers, particularly in the setting of relapsed disease following chemotherapy.
Although initial reports suggested a possible role for HSCT in breast cancer, subsequent studies do not support a role for this disease.
Relapsed prostate cancer is often treated with systemic endocrine and chemotherapeutic agents; there is no established role for HSCT here.
Relapsed liver cancer is often treated with ablative therapies or systemic targeted and chemotherapeutic agents; there is no established role for HSCT here.
Relapsed kidney cancer is often treated with systemic targeted therapies; there is no established role for HSCT here.
Day 7 Pediatrics Q&A
On the seventh day of 12 Days of Q&As MedStudy gave to me.... A question from the Infectious Disease section of the Peds Q&As!
A male born at 33 weeks of gestation is admitted to the neonatal intensive care unit following a vaginal delivery, complicated by premature rupture of membranes and maternal fever. Treatment for presumed sepsis is initiated following laboratory evaluation, which subsequently includes blood and cerebrospinal fluid (CSF) cultures positive for Listeria monocytogenes.
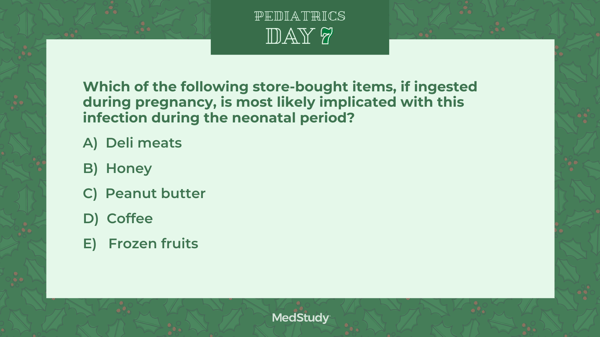
Answer is A- Deli meats
Listeriosis, which is caused by Listeria monocytogenes, is primarily a foodborne infection that may be asymptomatic or cause an influenza-like illness during pregnancy. Recommendations for prevention of foodborne listeriosis include avoiding unpasteurized milk, dairy products, and soft cheeses; undercooked and unwashed foods; prepared meats (e.g., deli meats, hot dogs, luncheon meats); and refrigerated smoked seafood. Pasteurization of dairy products kills the bacteria.
Transplacental transmission or ascending spread from vaginal colonization may cause spontaneous abortion or stillbirth, or may be associated with premature delivery. Neonatal illnesses can have an early-onset or late-onset disease similar to that of group B streptococcal infections. Early-onset disease has a mortality rate of 20–30% and is characterized by pneumonia and septicemia. An erythematous rash with small, pale papules, characterized histologically by granulomas (termed “granulomatosis infantisepticum”) can occur in severe newborn infection. Late-onset disease (from 8-30 days of age) usually results in meningitis and is associated with a mortality rate of 10–20%.
Listeriosis is clinically indistinguishable from neonatal sepsis and meningitis caused by other organisms such as group B streptococci, Escherichia coli, enterococci, and other enteric organisms. Patients typically have an elevated WBC count, often with 10–20% monocytes. The CSF cell count is high (> 500/mL) with a predominance of polymorphonuclear neutrophils or monocytes. On Gram stain of CSF fluid, short gram-positive rods may be seen. During evaluation for presumed neonatal sepsis, Listeria monocytogenes may be mistaken for a contaminant because of its morphologic similarity to diphtheroids and streptococci. Initial therapy with intravenous ampicillin and gentamicin is recommended for both early-onset and late-onset disease. It is more effective than ampicillin alone, because gentamicin has a synergistic effect with ampicillin and lowers the minimum inhibitory concentration.
Peanut butter is not associated with listeriosis. Salmonella has been associated with improperly manufactured peanut butter.
Consumption of coffee and frozen fruits (that have been prewashed before freezing) are not commonly associated with listeriosis. (Unpasteurized milk/dairy products and unwashed frozen fruit have been documented as being contaminated with Listeria, Salmonella, or Escherichia coli when improperly processed.)
Consumption of honey (by the infant, not the pregnant woman) can be associated with infant botulism; therefore, children < 12 months of age should not be fed honey.
Day 8 Internal Medicine Q&A
On the eighth day of 12 Days of Q&As MedStudy gave to me.... A question from the Oncology section of the IM Q&As!
-png.png?width=600&name=day%208%20tw%20(1)-png.png)
Answer is B - Gross lower gastrointestinal bleeding in a 60-year-old man
Lower gastrointestinal bleeding is an indication for colonoscopy.
Staphylococcus epidermis bacteremia is not associated with any classic condition requiring a colonoscopy.
Irritable bowel syndrome (IBS; i.e., pain that is relieved with defecation in a patient with anxiety) and IBS-like symptoms without alarm signs (i.e., alternating diarrhea and constipation) do not require colonoscopy. Diagnose IBS by ruling out other diseases, particularly celiac disease, lactose intolerance, bacterial overgrowth, and excessive sorbitol intake, and by looking for the characteristic symptoms defined by the International Classification for Irritable Bowel Syndrome, commonly called the Rome III criteria.
Iron-deficiency anemia in a young woman with heavy menses is not an indication for colonoscopy.
Day 9 Pediatrics Q&A
On the ninth day of 12 Days of Q&As MedStudy gave to me.... A question from the Ophthalmology and ENT section of the Peds Q&As!
-png.png?width=600&name=day%209%20peds%20tw%20(1)-png.png)
Answer is A - Untreated strabismus leads to loss of visual acuity.
Strabismus is intermittent or continuous misalignment of one or both eyes. If left untreated, it can lead to amblyopia (loss of visual acuity). Early detection and treatment leads to better long-term outcomes.
Esotropia is the most common form of strabismus in childhood. Esotropia is defined as an inward deviation of the eye towards the nose and is often referred to as "cross-eyed." Exotropia is an outward deviation of the eye. Deviation upward is “hypertropia,” and deviation downward is “hypotropia.” The most effective treatment, patching the better eye, forces the brain to use the eye with poor vision. While patching may not correct the eye crossing, it can improve vision of the affected eye.
Clinicians can detect strabismus on exam with simple tests, such as the corneal light reflex, the cover test, the cover/uncover test, and the Brückner test. These tests should be used together for a more accurate evaluation. However, if the clinical exam is normal, a history of misalignment from the parent/guardian is sufficient to warrant a referral to an ophthalmologist.
Day 10 Internal Medicine Q&A
On the tenth day of 12 Days of Q&As MedStudy gave to me.... A question from the Psychiatry section of the IM Q&As!
A 30-year-old woman has a 3-year history of irritable mood, hypersomnia, and poor concentration. She reports feeling depressed most of nearly every day. She has never felt manic or had such symptoms. She has tried several antidepressant medications without significant change in mood or outlook.
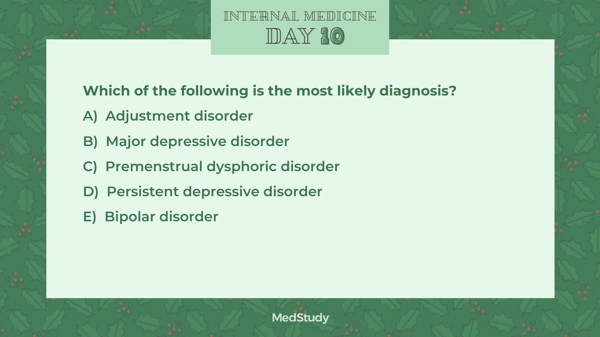
Answer is D - Persistent depressive disorder
DSM-5 combined chronic major depression and dysthymic disorder into persistent depressive disorder (PDD). PDD consists of a persistent, long-term change in mood that generally is less intense but more chronic than occurs in major depressive disorder (MDD). The symptoms of PDD may not be as severe, but they can cause more psychosocial impairment. Per DSM-5 criteria, a PDD diagnosis requires that a depressed mood must occur for most of the day, occur more days than not, and last at least 2 years. Depressive symptoms must be accompanied by at least 2 of the following:
Poor appetite or overeating
Insomnia or hypersomnia
Low energy or fatigue
Low self-esteem
Poor concentration
Difficulty with making decisions
Feelings of hopelessness
This is very difficult to differentiate from MDD, which has to have at least 5 of the following for most of the day, every day, for the past 2 weeks:
Depressed mood
Loss of interest or pleasure in usual activities
Significant weight loss or gain
Insomnia or hypersomnia
Psychomotor agitation or retardation
Fatigue or loss of energy
Feelings of worthlessness or excessive or inappropriate guilt
Diminished ability to think or concentrate
Recurrent thoughts of suicide or death
Many patients with PDD can enter into periods of MDD, a condition known as “double depression.” These patients can respond to treatments but are more likely to experience relapses of MDD. A clue for PDD are buzzwords like “gloomy outlook on life” or “an underlying sense of inadequacy.”
Premenstrual dysphoric disorder refers to cyclic periods of mood disorder that occur the week prior to menses and resolve within a few days of menses.
Adjustment disorder refers to a situational depression related to an inability to cope with a particular stressful event (e.g., death of a loved one, loss of a job, moving). Unlike PDD, adjustment disorder is related to an outside stressor and typically resolves once the individual learns to cope with the new situation.
Bipolar disorder is a unique mental disorder characterized by periods of depression interspersed with periods of elevated mood (mania or hypomania). This patient has never had an episode of manic behavior to suggest a diagnosis of bipolar disorder.
Day 11 Pediatrics Q&A
On the eleventh day of 12 Days of Q&As MedStudy gave to me.... A question from the Preventive Pediatrics section of the Peds Q&As!
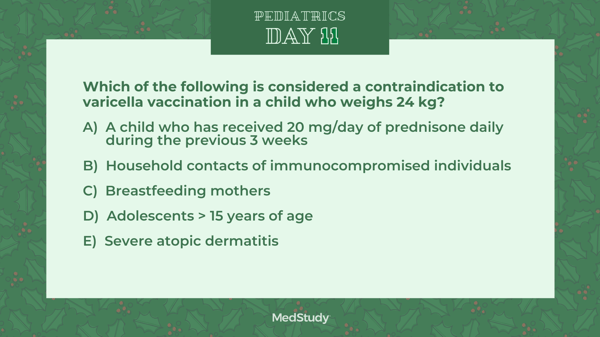
Answer is A - A child who has received 20 mg/day of prednisone daily during the previous 3 weeks
Individuals who are receiving systemic corticosteroids (≥ 2 mg/kg/day of prednisone or ≥ 20 mg/day of prednisone) for ≥ 2 weeks should not receive the varicella vaccine for at least 1 month after discontinuation of treatment.
Additional contraindications to the vaccine include severe allergic reaction (i.e., anaphylaxis), severe immunosuppression, pregnancy (or possibility of pregnancy within 4 weeks), and recent administration of immunoglobulin. Of note, the varicella vaccine is not contraindicated in all HIV-infected children; rather, varicella vaccine should be considered for HIV-infected children with a CD4+ T-lymphocyte percentage of ≥ 15%.
The live-attenuated varicella vaccine is routinely recommended at 12–15 months of age. A 2nd dose of vaccine is recommended at 4–6 years of age but may be administered at an earlier age (i.e., during a varicella outbreak) providing a 3-month interval has passed since administration of the 1st dose. The risk of a febrile seizure in toddlers is slightly higher 1–2 weeks after immunization with the combined measles, mumps, rubella, and varicella (MMRV) vaccine when compared to the monovalent varicella vaccine. However, MMRV generally is preferred for the 2nd dose at 4–6 years of age to minimize the number of injections. MMRV is not approved for those > 12 years of age.
Household contacts of immunocompromised people should be immunized to decrease the likelihood that wild-type varicella-zoster virus will be introduced in the household.
Breastfeeding is not a contraindication to varicella vaccination, but babies in this situation do not seroconvert.
Previously unimmunized adolescents ≥ 13 years of age should receive 2 doses of monovalent varicella vaccine, separated by at least 28 days (3 months if < 13 years).
Varicella infection is often more severe in patients with atopic dermatitis; however, this disorder is not a contraindication to the varicella vaccine.
Day 12 Internal Medicine Q&A
On the tenth day of 12 Days of Q&As MedStudy gave to me.... A question from the Cardiology section of the IM Q&As!
A 28-year-old male was found to have elevated triglycerides at 1,200 mg/dL on fasting lipid panel, which was consistent with a diagnosis of familial hyperchylomicronemia.
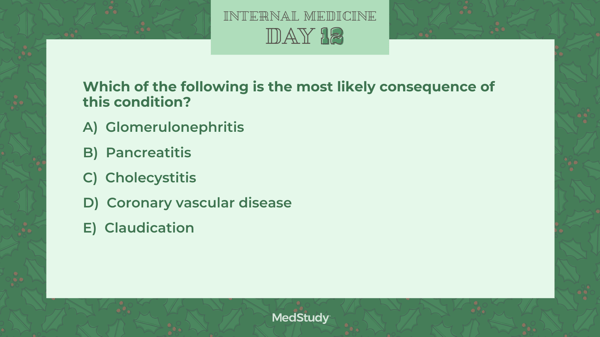
Answer is B - Pancreatitis
Familial hyperchylomicronemia (hypertriglyceridemia) is manifested by markedly elevated triglycerides, with the predominant elevation coming from increased chylomicrons. Pancreatitis is recognized to occur more frequently in patients with the marked triglyceride elevation. The higher the triglyceride levels, the greater the risk of developing pancreatitis.
Several renal diseases can cause secondary hypertriglyceridemia, but elevated triglyceride levels do not directly lead to renal parenchymal disease.
No direct relationship between hypertriglyceridemia and cholecystitis has been reported in this condition.
The impact on cardiovascular risk is variable but is significantly less than would be expected, based on the level of elevation that is commonly seen in these patients.
Similar to coronary vascular disease, peripheral vascular disease and claudication are not expected in familial hypertriglyceridemia because it is not typically associated with atherosclerosis.
Make sure you're following us on Facebook, Twitter, and Instagram to see weekly Q&As! And, if you liked these detailed explanations, make sure you start self-testing with your own Internal Medicine Q&A bank or our Pediatrics Q&A bank.


